Reptile Dental Care
Authored by Christina Miller RVT, BSc, of Companion Animal Hospital, Canada.
Veterinary practices across North America participate in National Pet Dental Health month which is in February by encouraging pet owners to learn about how important good oral health is in their companion animals, like it is in people. But, why care if you have a pet reptile? Reptiles don’t get dental disease…or do they?
Teeth vary greatly in size, form, and function across the animal kingdom, suiting an organism’s lifestyle, diet, and even species-specific behaviours in some cases. While we have some evidence that dental or periodontal disease occurs in wild animals (Steenkamp and Gorrel 1999, Van Valkenburgh 1988), we certainly do see a different progression of dental disease in companion as well as zoo animals. The reasons for this happening can be complex and vary greatly with different species, and in some cases the exact reason is still unknown. This region of medicine has grown in the past decade for reptiles, and more veterinarians are recognizing dental disease and periodontal disease in their reptilian patients.
Understanding dental anatomy

All-in-all, teeth generally have a similar basic structure. Let’s take a look at this structure in most vertebrates (Gorrel and Derbyshire 2005), see Figure 1 for a summary of a normal tooth’s anatomy:
- Teeth may be split into the crown (above the gumline) and the root(s) (below the gumline).
- Most of the tooth consists of dentine, that is covered by tough enamel above the gumline (the crown), and cementum below the gumline (the root).
- Pulp in the centre of the tooth contains vital tissue: Nerves and the tooth’s blood supply are located here.
- The periodontium or periodontal tissue makes up the tissues that surround the tooth, attaching the tooth to the jaw.
- Alveolar bone is the ridge of jaw bone that meets the tooth, supporting it. In many species, the alveolar bone has a deep depression, the alveolar socket, which surround the root of the tooth.
- The periodontal ligament is tough connective tissue that attaches the tooth root to the bony alveolar socket, and allows very slight movement of the tooth. This adds some element of “shock absorption” to the tooth’s firm structure.
- The gingiva (commonly known as “gums”) surrounds the teeth as well as the margin of the alveolar bone. Part of the gingival tissue is “free,” not attached to the underlying bone but creates a small flap of tissue surrounding the teeth: The pocket formed between the tooth and attached gum tissue is called a sulcus. Most of the gingival tissues are firmly attached to the underlying bone.
We have many other terms used to describe the dentition of different species:
- Polyphyodont dentition means that the teeth are replaced throughout the animal’s lifetime as they are lost to the wear and tear of capturing prey or fighting (Buchtova et al. 2012), at differing intervals for replacement. Good examples of polyphyodonty in vertebrates include crocodilians (LeBlanc et al. 2013), some lizards such as geckos (Handrigan et al. 2010), snakes (O’Malley 2005), and a few mammals such as manatees (MCC 2010).
- Diphyodont dentition means that the animal has a set of deciduous or “baby” teeth that are replaced by permanent or “adult” teeth (Gorrel and Derbyshire 2005). This is the most common type of tooth replacement in mammals.
- Monophyodont dentition means that the animal has a single set of teeth that are not replaced if damaged or lost (Yadav and Khanna 2005). Some lizard groups do not replace teeth after they reach adulthood (O’Malley 2005).
Reptiles have varying tooth anatomy depending on their evolutionary roots.
- Crocodilians have thecodont dentition, where the teeth sit in a deep, bony socket like in mammals (O’Malley 2005), however the periodontal attachment is not as well-developed as in mammals (McIntosh et al. 2002).
- Most lizards have pleurodont dentition. The teeth are attached to the lingual (inner) edge of the alveolar bone, and sit in a groove that is not as well-defined as a socket. The periodontal ligament is poorly developed to non-existent, and instead the tooth is ankylosed (a form of bony fusion) to the jaw bone (O’Malley 2005).
- A few lizard groups, including family Agamidae (bearded dragons, water dragons, and relatives) and Chameleonidae (the true or “Old World” chameleons), as well as snakes, have acrodont dentition. The jaw bone has a tall, narrow alveolar crest covered by thin gingival tissue, and the tooth is ankylosed to the top of this crest. Acrodont dentition is the most clinically relevant type of tooth structure in veterinary medicine, as some of these features seem to create a predisposition towards developing periodontal disease. We will explore this concept further, below.
Development of periodontal disease
The vast majority of dental problems are forms of periodontal disease, or disease affecting the tissues surrounding the actual tooth as described above (Gorrel and Derbyshire 2005). In our canine and feline companions, it is one of the most common diseases that we see in practice, with most patients over the age of three years having some form of periodontal disease (AVDC 1988).
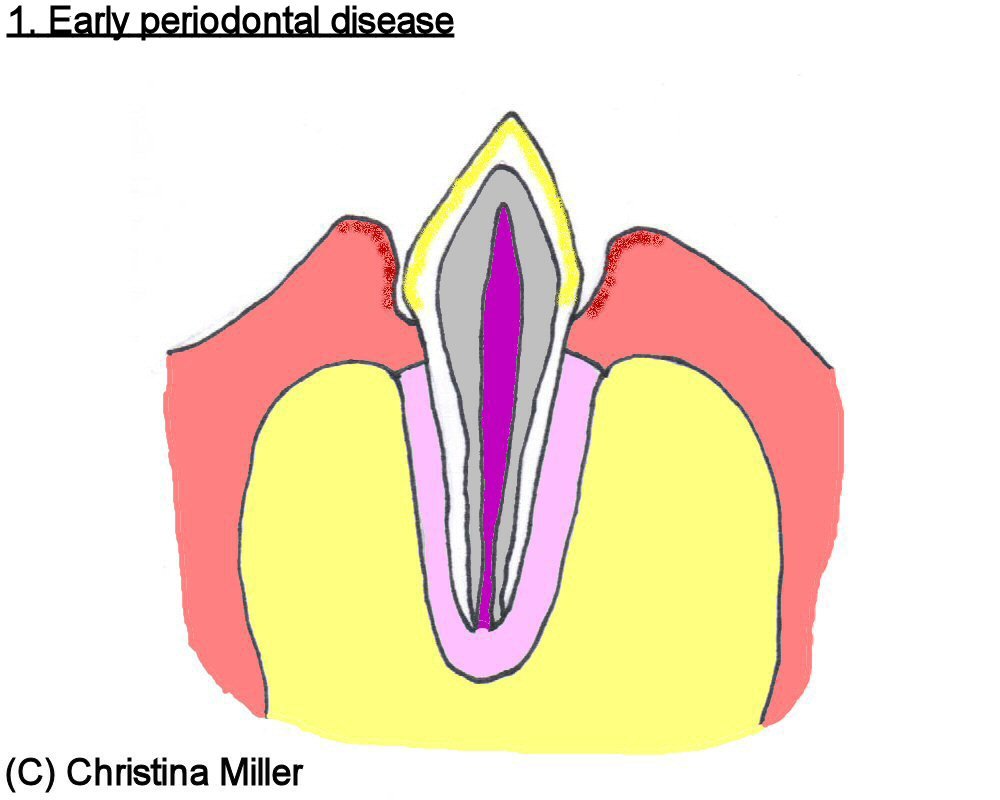
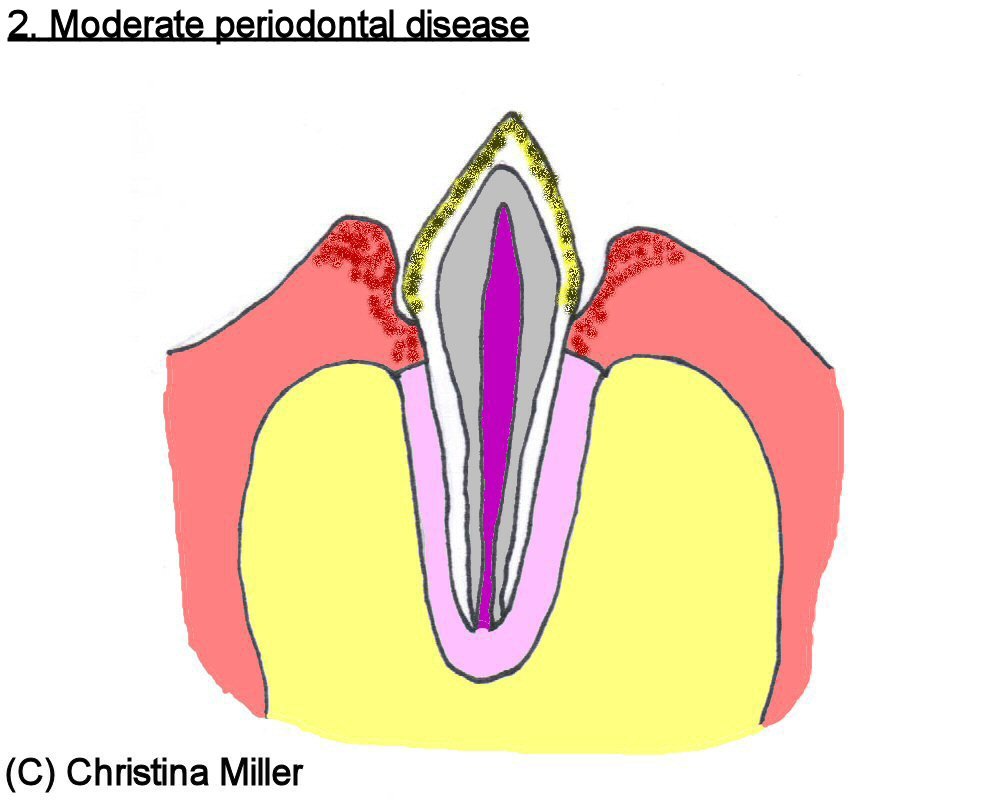
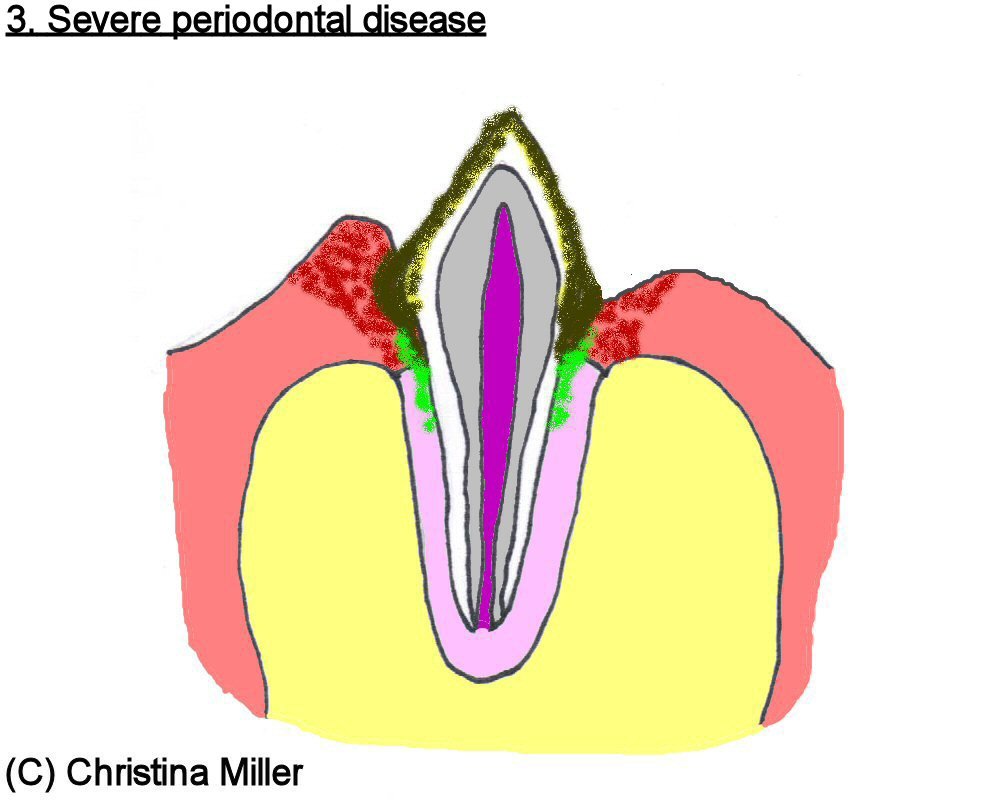
These pathologies have a pretty standard progression. Bacteria that naturally live in the mouth, their excretions, food debris, dead white blood cells, and normal compounds found in the saliva will collect on teeth into a biofilm, called plaque. Plaque is the “soft” material that we remove from our teeth with regular brushing. Plaque that is not regularly removed will combine with minerals naturally found in saliva, and harden into calculus or tartar. If calculus is not removed (by a professional dental cleaning), new plaque layers on top and will form layer after layer of calculus. This acts as a substrate for bacteria that become disease-causing. We have many terms to describe the disease directly and indirectly caused by these bacteria (Gorrel and Derbyshire 2005).
Gingivitis is the inflammation of gingival tissue. This appears as reddened, swollen gums, and even bleeding of the margin of gum tissue that meet the tooth surface. Inflammation or hyperplasia (where the tissue “overgrows” as a result of plaque accumulation) of the gum tissue can result in a widening of the pocket between the gums and tooth, or creating a larger “pseudo-pocket” in the case of gingival hyperplasia, allowing even more plaque and bacteria to infiltrate the periodontal tissue. With gingivitis, there is no loss of the tooth’s attachment to underlying bone, and gingivitis is reversible with good oral hygiene (Gorrel and Derbyshire 2005).
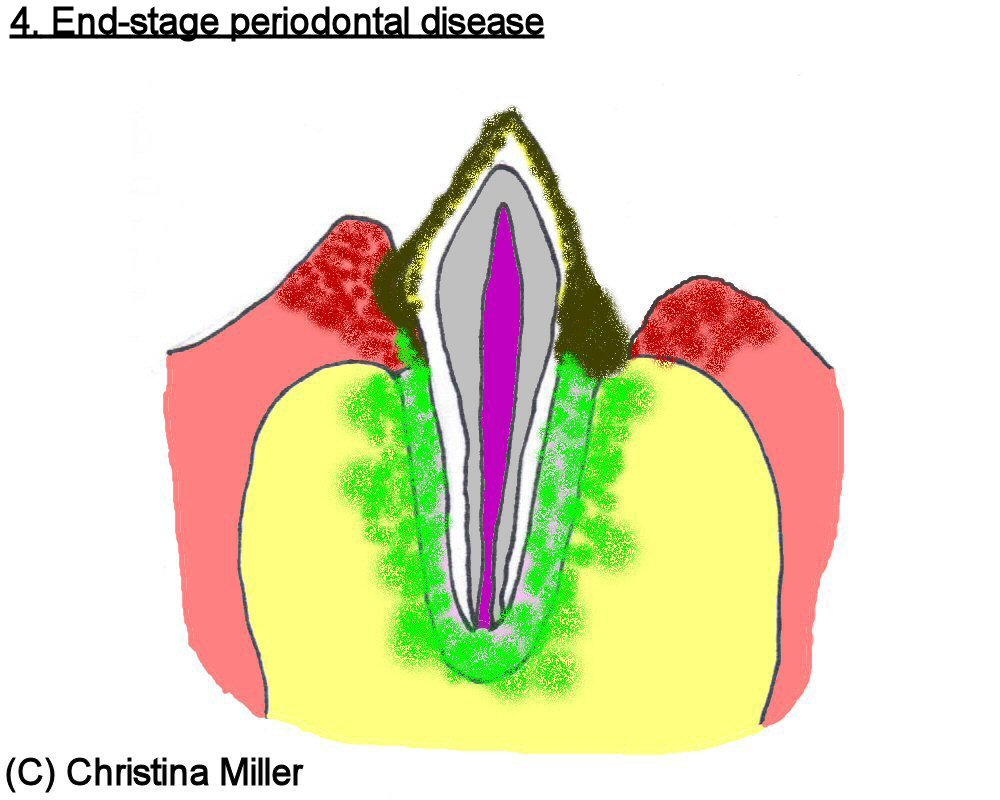
Untreated gingivitis may develop into periodontitis, where the bone and ligament that anchor the tooth in place become infected and gradually destroyed. This results in the tooth becoming mobile in its periodontal attachment, becoming a vicious cycle where a “wobbly” tooth allows for more subgingival plaque and bacteria to accumulate, resulting in a worsening periodontal infection, etc. This can eventually lead to tooth root abscessation and even a bone infection, termed osteomyelitis. Periodontitis is irreversible. In veterinary medicine, teeth with significant periodontal destruction are typically extracted (surgically removed) since they are a source of pain and infection that can result in an infection of the jaw bone (Gorrel and Derbyshire 2005). These bacteria are also “seeded” into the bloodstream, and infections in vital organs such as the heart, liver, and kidneys can be traced back to poor oral health (De Bowes et al. 1996).
Figures 3 through 6 illustrate the progression of periodontal disease.
Periodontal Disease and Reptiles
Periodontal disease in reptiles was first described in 1994 (McCracken and Birch 1994). Periodontal disease occurs in reptiles for a variety of reasons, but as mentioned above, lizards with an acrodont dentition are the most predisposed. Recall these lizards have a tall, thin crest of bone covered with a thin epithelial layer that is different from gingival tissue (Boyer 2015). This seems to allow for more bacterial colonization compared to regular gingival tissue (Boyer 2015).

Chinese Water Dragon (Physignathus concincinus) with early periodontal disease, there is some mild accumulation of calculus along the teeth.
When this layer is damaged, either from “wear and tear” over a long lifetime, or from calculus deposition, bacteria can easily invade the bone of the jaw causing osteomyelitis (Simpson 2015). While bacterial infection is common (Simpson 2015), fungal osteomyelitis has also been documented (Heatley et al. 2001). We do not grade periodontal disease the same as we do in mammalian companion animals, however a grading system has been proposed (Simpson 2015) and can only help veterinarians better communicate. Signs of periodontal disease can include a loss of appetite or difficulty apprehending food, pain when chewing, bleeding from the oral cavity, swelling of the upper and lower jaws, and some patients show absolutely no clinical signs but may still have significant disease (Simpson 2015).

The same animal as in Figure 7; this is a radiograph of the mandible (lower jaw). The yellow arrow indicates a region of osteomyelitis, or bone infection.
Treatment varies depending on the severity of disease. Your veterinarian may require testing such as oral radiographs (x-rays, which may need to be taken under sedation or general anesthesia), bloodwork to obtain a general picture of your pet’s health, and potentially a culture of the infected tissues to better guide antibiotic selection. Severe cases where the infection has invaded the bone typically require surgery to remove (debride) the infected tissue, allowing for a “clean slate” for the body to start healing.

This Leopard Gecko (Eublepharis macularius) had such a severe oral infection that he lost all of his teeth, and as a result could not shed effectively. This resulted in eye infections and constricted toes in this patient.
The reasons for significant periodontal disease in captive acrodont lizards is not certain, however the predominant theory is that captive diets may not provide enough roughage compared to wild diets (Simpson 2015). The role of other nutritional or systemic disease cannot be ignored (Simpson 2015). More research and review is needed in this area to better understand how we can prevent periodontal disease. Talk to your veterinarian to learn more about treating periodontal disease in your pet.

This Green Anole (Anolis carolinensis) is suffering from severe osteomyelitis of the jaw. This likely did not begin as periodontal disease, but may have been a result of a rostral abrasion during transport. Early treatment may have saved this patient.
References
American Veterinary Dental College (AVCD). 1988. “Periodontal Disease.” <http://www.avdc.org/periodontaldisease.html> Accessed 19-Feb-2017
Boyer, TH. 2015. “Diseases of Bearded Dragons.” Proceedings of the Pacific Veterinary Conference 2015.
Buchtova, M, J Stembirek, K Glocova, E Matalova, AS Tucker. 2012. “Early Regression of the Dental Lamina Underlies the Development of Diphyodont Dentitions.” Journal of Dental Research, 91(5):491-498.
De Bowes, LJ, D Mosier, E Logan, et al. 1996. “Association of periodontal disease and histologic lesions in multiple organs from 45 dogs.” Journal of Veterinary Dentistry 13(2):57-60.
Gorrel, C and S Derbyshire. 2005. Veterinary Dentistry for the Nurse and Technician. Elsevier Limited, London, United Kingdom.
Handrigan, GR, KJ Leung, JM Richman. 2010. “Identification of Putative Dental Epithelial Stem Cells in a Lizard with Life-long Tooth Replacement.” Development and Stem Cells, 137(2010):3545-3549.
Heatley, J, MA Mitchell, J Williams, JA Smith, TN Tully. 2001. “Fungal Periodontal Osteomyelitis in a Chameleon, Furcifer pardalis.” Journal of Herpetological Medicine and Surgery, 11(4):7-12.
Klaphake, E. 2015. “Reptile Oral Medicine.” American Association of Zoo Veterinarians Conference 2015.
LeBland, ARH, RR Reisz, L Viriot. 2013. “Peridontal Ligament Cementum, and Alveolar Bone in the Oldest Herbivorous Tetrapods, and Their Evolutionary Significance.” Public Library of Science ONE, 8(9):e74697.
Marshall Cavendish Corporation (MCC). 2010. Mammal Anatomy: An Illustrated Guide. Cavendish Square Publishing, New York, U.S.A.
McIntosh, JE, X Anderton, L Flores-De-Jacoby, DS Carlson, CF Shuler, TGH Diekwisch. 2002. “Caiman periodontium as an intermediate between basal vertebrate akylosis-type attachment and mammalian “true” peridontium.” Microcopy Research Technique, 59:449-459.
McCracken, H and CA Birch. 1994. “Periodontal disease in lizards- a review of numerous cases.” Proceedings of the American Association of Zoo Veterinarians, 108-114.
O’Malley, B. 2005. Clinical Anatomy and Physiology of Exotic Species.
Simpson, S. 2015. “Dragon Breath… Periodontal Disease in Central Bearded Dragons (Pogona vitticeps).” Proceedings of Association of Avian Veterinarians Australasian Committee-Unusual Pets and Avian Veterinarians.
Steenkamp, G and C Gorrel. 1999. “Oral and dental conditions in adult African wild dog skulls: a preliminary report.” Journal of Veterinary Dentistry, 16(2):65-68.
Van Valkenburgh, B. 1998. “Incidence of tooth breakage among large, predatory mammals.” American Naturalist, 291-302.
Yadav, PR and DR Khanna. 2005. Biology of Mammals. Discovery Publishing Group, Limited, New Delhi, India.